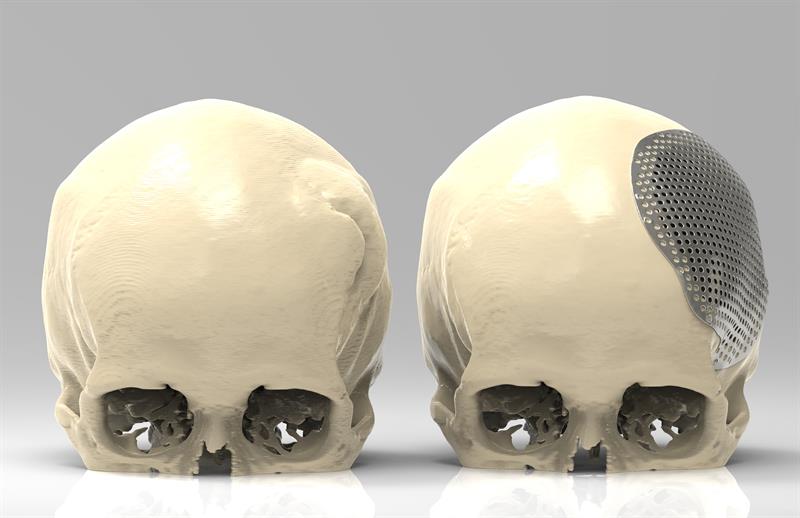
PSIs can be produced by additive manufacturing (AM) in several different materials for medical applications, and it should be remembered that AM is still a relatively new technology for the medical sector.
AM offers several benefits over traditionally made implants, including fewer geometric limitations on implant design. Implants created using AM technology are built in layers from powdered metal resulting in fewer restrictions on what can be manufactured. What were extremely complex structures are straightforward to manufacture using AM.
Adopting AM implants
AM implants are now commonly used in Southmead Hospital, Bristol, for craniomaxillofacial (CMF) procedures.
Prior to adopting the AM implant technology, the prosthetics team would produce a 3D model of the patient’s skull from a mould made of dental plaster and stone. This would be used to press a sheet of titanium to form the implant.
Additive manufacturing eliminates the need to make a mould as the implant is produced on an AM machine using digital data, speeding up both the design and manufacture processes.
Models required for surgical planning can also be printed from a patient’s CT data and can be integrated with surgical planning software to produce a digital 3D visualisation.
From my experience, I have found it very straightforward to adapt to the new technology. However, it is important that work continues to develop on more advanced software packages, as current options require highly trained and experienced members of staff to do the design. In Southmead Hospital, we use a platform called Geomagic Freeform Plus to design the implants.
In future, software packages such as ADEPT, available from Renishaw, will make the design process even more straightforward. ADEPT is computer-aided design software that has been specifically created for the rapid design of craniomaxillofacial, PSIs by metal 3D printing.
Once an implant has been designed, the hospital can send the design to a third-party company, such as Renishaw, for manufacture. Additive manufacturing produces precise guides, models and implants to the surgeon’s specification, which can improve the outcome for the patient as it allows for a quicker procedure, less surgery time and an accurate fit with good aesthetics.
Opening doors
Additively manufactured implants are helping to improve treatment processes and decrease procedure revision numbers and times, which can also reduce costs for the NHS and provide better patient outcomes.
There can be greater benefits in more complex cases, however AM technology can still help to streamline surgery for less complex procedures. Surgeons are able to carry out careful pre-planning, which means they have reduced spans of problem solving during surgery.
The implants offer improved treatment processes for patients. One major advantage is the reduction in the number of procedures a patient may need. Traditionally, if a patient had a particular cranium tumour, a surgeon would first have to remove the tumour and close the wound. The patient would then require further CT scans to determine the size of the cranial plate needed. The surgeon would then perform a second procedure to insert the implant.
By using surgical planning software and AM technology, the surgeon can pre-plan before surgery. Custom AM surgical guides and implants are also created before surgery. The guides allow the surgeon to remove the tumour and place the cranial plate, in one surgical procedure, with precision.
Improved surgical planning streamlines the surgery process leading to a reduction in theatre time, which in turn can reduce NHS costs.
In order for the technology to reach its potential, industry and healthcare need to work together to progress it further by developing a body of evidence demonstrating the efficacy and benefits both to the hospital and patients.
It is also important that early adopters of the technology, such as the team in Southmead Hospital, apply their knowledge to drive the technology forward to also reinforce that the additive manufacturing of implants could improve not just patient care but could also be of financial benefit to health services.
About the author:
Amy Davey is a reconstructive scientist at North Bristol NHS Trust
Replacement jaw implants have been made to treat temporomandibular joint endoprostheses, which severely reduces many facial senses. Typically, implants are made from medical Grade-5 titanium alloy Ti6Al4V by direct laser metal sintering. For its surgical guides and implant models, a biocompatible polymer PA 2200 (also known as Nylon-12) is selective laser sintered. Medical CT scans are the basis for preparing the CAD model, while inspection of AM parts is carried out with a Nikon Metrology industrial, high voltage, micro-CT scanner. Milda Jokymaitytė, clinical engineer at Ortho Baltic explains: “To create anatomical models, 3D reconstruction engineers use the patient’s radiological data to perform a 3D reconstruction.” A Nikon Metrology XT H 225 micro-CT scanner is used to monitor the quality of the final part and inspect the external geometry and internal structure. The inspection uses a 225kV micro-focus source that non-destructively reveals any voids, cracks and other defects of the complex internal features of the AM components. Domantas Ozerenskis, product quality manager at Ortho Baltic, adds: “Micro-CT scanning is the only way to non-destructively check for voids and cracks inside a part. “We considered a coordinate measuring machine, but it is inconvenient for taking non-parametric measurements and there is no possibility for inner structure investigation. “The internal quality of implants is very important, as it determines the part’s mechanical strength.” After 3D metal printing, post-processes such as sandblasting and polishing can remove thick surface layers up to 200µm – even more in the case of other manual processes. It means micro-CT data can also help adjust CAD models toreflect a part’s final geometry. |








 CT scan data drives implant design
CT scan data drives implant design


